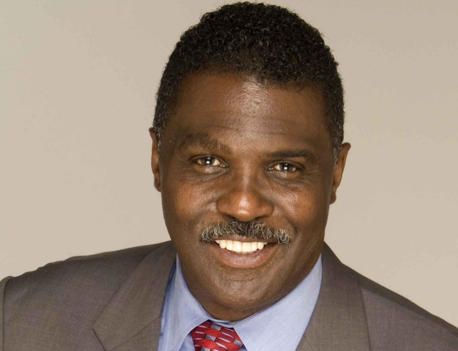
By Glenn Ellis
There’s clearly a connection between substance abuse and mental health disorders!
The National Bureau of Economic Research (NBER) reports that there is a “definite connection between mental illness and the use of addictive substances” and that mental health disorder patients are responsible for the consumption of: 38 percent of alcohol; 44 percent of cocaine; and 40 percent of cigarettes.
Often, certain drugs can create problems that trigger mental health symptoms. In other cases, substances can create those symptoms like paranoia, delusions or depression while the person is under the influence of the drug. When these symptoms last after the drugs wear off, then it can indicate a co-occurring mental health disorder.
Doctors say they are increasingly seeing patients from all walks of life who suffer from a combination of substance abuse and mental health problems. Experts estimate that at least 60 percent of people battling one of these conditions are battling both.
Mental health problems are common in the U.S. An estimated one in five adults in the U.S. suffers from a diagnosable mental disorder, according to the National Institute of Mental Health.
When there is a biological or genetic vulnerability to any type of mental health problem, regardless of how big or small, substance use often triggers the onset of that problem. The substance is not really causing the problem, but it can be a precipitating factor that causes the condition to manifest.
Whether the mental health problem – or the drug use – came first, doctors say that good mental health can’t prevail until both problems are treated.
Dual diagnosis (also referred to as co-occurring disorders) is a term for when someone experiences a mental illness and a substance use disorder simultaneously. Either disorder — substance use or mental illness — can develop first. People experiencing a mental health condition may turn to alcohol or other drugs as a form of self-medication to improve the symptoms they experience. However, research shows that alcohol and other drugs worsen the symptoms of mental illnesses.
Unfortunately, the dual approach is still considered somewhat specialized, and frequently only available in pricey private hospitals. The next best thing, say experts, is to integrate patient care among the professionals dealing with each part of the illness.
The best treatment for dual diagnosis is integrated intervention, when a person receives care for both their diagnosed mental illness and substance abuse. The idea that “I cannot treat your depression because you are also drinking” is outdated – current thinking requires both issues be addressed.
It can be difficult to diagnose a substance abuse problem and a co-occurring mental health disorder. It takes time to tease out what might be a mental disorder and what might be a drug or alcohol problem. The signs and symptoms also vary depending upon both the problem and the type of drug being abused. For example, the signs of depression and marijuana abuse could look very different from the signs of schizophrenia and alcohol abuse. However, there are some general warning signs that you may have a co-occurring disorder.
Denial
Complicating a dual diagnosis is denial. Denial is common in substance abuse. It’s often hard to admit how dependent you are on alcohol or drugs or how much they affect your life. Denial frequently occurs in mental disorders as well. The symptoms of depression or anxiety can be frightening, so you may ignore them and hope they go away. Or you may be ashamed or afraid of being viewed as weak if you admit you have a problem. But substance abuse and mental health issues can happen to any of us. And admitting you have a problem and seeking help is the first step on the road to recovery.
When you have both a substance abuse problem and a mental health issue such as depression, bipolar disorder, or anxiety, it is called a co-occurring disorder or dual diagnosis. Dealing with substance abuse, alcoholism, or drug addiction is never easy, and it’s even more difficult when you’re also struggling with mental health problems. But there is hope. There are plenty of treatments and steps you can take to help you on the road to recovery. With the right support, self-help, and treatment, you can overcome a co-occurring disorder, reclaim your sense of self, and get your life back on track.
Make sure that the program is appropriately licensed and accredited, the treatment methods are backed by research, and there is an aftercare program to prevent relapse. Additionally, you should make sure that the program has experience with your particular mental health issue.
Veterans deal with additional challenges when it comes to co-occurring disorders. The pressures of deployment or combat can exacerbate underlying mental disorders, and substance abuse is a common way of coping with unpleasant feelings or memories. Often, these problems take a while to show up after a vet returns home and may be initially mistaken for readjustment.
The same applies to inner-city youth who experience or witness gun violence, resulting in PTSD. Rates in this population is often higher than in veterans. Untreated co-occurring disorders can lead to major problems at home and work and in your daily life, so it’s important to seek help.
Remember, I’m not a doctor. I just sound like one.
Take good care of yourself and live the best life possible!
The information included in this column is for educational purposes only. It is not intended nor implied to be a substitute for professional medical advice.
Glenn Ellis is a health columnist and radio commentator who lectures, nationally and internationally on health related topics. Listen to Glenn, on radio in Birmingham or V94.9, Sundays at 7:50 p.m., or visit: www.glennellis.com.