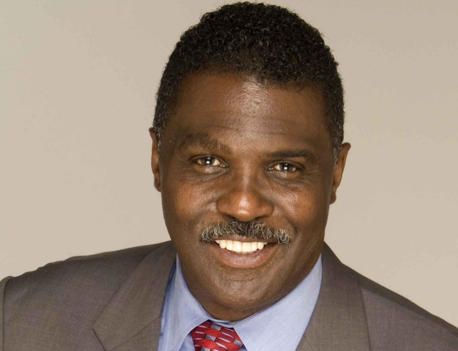
By Glenn Ellis
Heart Failure is a scary term.
The words can be misleading. The heart is a muscle that pumps blood to the other organs of the body, but “heart failure” doesn’t mean the heart has stopped working. It means it can’t pump properly – so it doesn’t fully support the body’s need for blood and oxygen. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently.
Heart Failure is one of the most common reasons people over the age of 65 are hospitalized. It can get worse over time and can even lead to death. It is more common, not only in people who are 65 years old or older but also in African Americans; people who are overweight; and people who have had a heart attack. Men have a higher rate of heart failure than women.
The good news is that there are medicines proven to help manage it – along with healthy changes in lifestyle.
Heart failure often develops after other conditions have damaged or weakened your heart. However, the heart doesn’t need to be weakened to cause heart failure.
In heart failure, the main pumping chambers of your heart (the ventricles) may become stiff and not fill properly between beats. In some cases of heart failure, your heart muscle may become damaged and weakened, and the ventricles stretch (dilate) to the point that the heart can’t pump blood efficiently throughout your body.
Over time, the heart can no longer keep up with the normal demands placed on it to pump blood to the rest of your body.
At first, the heart tries to make up for this by “enlarging” itself. The heart stretches to contract more strongly and keep up with the demand to pump more blood. Over time this causes the heart to become enlarged.
The other way the heart attempts to keep up is by developing more muscle mass. The increase in muscle mass occurs because the contracting cells of the heart get bigger. This lets the heart pump more strongly, at least initially.
And lastly, the heart can sometimes just start pumping faster. This helps to increase the heart’s output.
There are a few other ways that the body tries to compensate. The blood vessels narrow to keep blood pressure up, trying to make up for the heart’s loss of power. The body then diverts blood away from less important tissues and organs (like the kidneys), and towards the heart and brain. These temporary measures mask the problem of heart failure, but they don’t solve it. Heart failure continues and worsens until these substitute processes no longer work.
Eventually the heart and body just can’t keep up, and the person experiences the fatigue, breathing problems or other symptoms that usually prompt a trip to the doctor.
Stage A: This is “pre–heart failure.” It means you’re at risk of more severe heart failure because you or someone in your family has diabetes, high blood pressure, early coronary artery disease, or family history of cardiomyopathy (a disease of the heart muscle). Treatment may include changing your diet, watching salt intake, reducing alcohol, increasing exercise, and possibly taking blood pressure medicines or other medication.
Stage B: This diagnosis is also early in the progression of heart failure. It means you already have some changes to the heart that could lead to heart failure. Your heart health also might be compromised because of blood pressure, but you don’t have classic symptoms of heart failure, yet. These people typically may have had a prior heart attack or they have some heart valve disease. Treatments could include those from stage A, as well as possible surgery or intervention as treatment for coronary artery blockage, heart attack, or valve disease.
Stage C: Individuals at this stage have been diagnosed with heart failure, and currently have or have previously had signs and symptoms of the condition, including shortness of breath, inability to exercise, swelling of their legs, or waking up short of breath after lying down.
Cardiac rehabilitation can help people with Stage C heart failure recover everyday functions and help them live longer lives and reduce symptoms.
Stage D: This is an advanced stage of heart failure and these patients are the sickest. People with this stage of heart failure should see a specialist to help determine the best course of treatment and which options are still on the table. It’s critical that they see a specialist within a few days of someone telling them they have stage D heart failure.
Regardless of the “stage” of heart failure, it is a chronic, long-term heart health condition that can get worse over time. But the sooner you begin making lifestyle changes to treat the condition, the better outcomes you can expect.
Remember, I’m not a doctor. I just sound like one.
Take good care of yourself and live the best life possible!
The information included in this column is for educational purposes only. It is not intended nor implied to be a substitute for professional medical advice. The reader should always consult his or her healthcare provider to determine the appropriateness of the information for their own situation or if they have any questions regarding a medical condition or treatment plan.
Glenn Ellis, is a Health Advocacy Communications Specialist. He is the author of Which Doctor?, and Information is the Best Medicine. A health columnist and radio commentator who lectures, nationally and internationally on health-related topics, Ellis is an active media contributor on Health Equity and Medical Ethics. For more good health information, visit: www.glennellis.com.